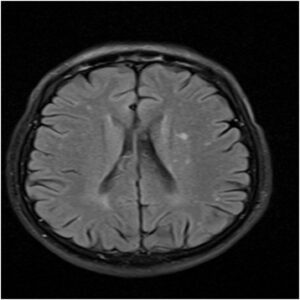
A recent study has established links between functional seizures aka non-epileptic seizures and structural abnormalities in our brains. These abnormal changes can only be identified on MRIs.
Non-epileptic seizures have always been associated with mental stressors like anxiety and PTSD (post-traumatic stress disorder). According to experts, the findings of this new study might help doctors in diagnosing functional seizures in their initial stages by eliminating possibilities of epilepsy. The study can also trigger the discovery of new treatment methods that would improve the quality of life by reducing the frequency of seizures.
What Are Functional Seizures?
Medical experts define functional seizures as a group of functional neurological symptoms. Health professionals use multiple synonyms for this condition. Examples include pseudo-epileptic seizures, pseudo-seizures, dissociative seizures, psychogenic seizures, conversion seizures, etc.
So many names for a single condition can make the situation confusing for patients. However, here, you must note that each name is describing one common thing i.e., attacks that resemble epileptic seizures but are not the results of abnormal electrical activities (epileptic activities) in the patient’s brain.
Recently obtained numbers suggest that two to three people out of every 10,000 individuals experience functional seizures. It has been found that almost 50% of patients, who need to visit hospitals with attacks that haven’t settled on their own, have functional seizures. These numbers make the condition moderately common.
How will you know whether you have an epileptic seizure, or you are experiencing a functional seizure? While most symptoms of the two conditions are common, there are some clues that indicate that you have functional seizures. They are:
- Prolonged and very frequent attacks
- Attacks that cause temporary loss of mobility
- Attacks that leave the patient emotionally upset
The common symptoms of functional seizures and epileptic seizures, on the other hand, are:
- Loss of bladder control
- Blackouts
- Collapsing (which may leave the patient severely injured)
Diagnosis of Functional Seizures
You must know that doctors never rely on just one event to conclude whether you are having functional seizures or any other form of seizure. Usually, the diagnosis is made based on long-term data obtained from multiple episodes of seizures.
When an individual experiences a blackout for the first time, the doctor manages to gather limited information from him or her. The patient becomes more mindful of the symptoms when the attacks start taking place again and again.
You must be able to describe the event in detail for the neurologist (treating you) to conclude that you have experienced a functional seizure. Only a proper description of the condition will allow the expert to spot the small but crucial aspects that differentiate functional seizures from epileptic seizures. Doctors even request family members of patients to capture photos and video recordings of attacks to make diagnosis easier.
Some Crucial Numbers
Most patients suffering from functional seizures get misdiagnosed with epilepsy and on average they need to wait for nine years to get the right diagnosis.
As untreated epileptic seizures can damage the brain permanently and even have fatal consequences, doctors tend to prescribe seizure medications despite not being sure of their diagnosis. However, eventually, around 10% of those patients turn out to be victims of functional seizures. Such misdiagnoses can have serious implications. Other than experiencing deterioration of symptoms of functional seizures, the patients can also suffer from debilitating side effects of epilepsy treatment.
However, things might soon change thanks to a study that has found that structural abnormalities in the human brain can trigger functional seizures. Read on to know more about the study.
The Study in a Nutshell
During the said study, researchers analyzed 650+ high-quality MRIs to compare the brain images of individuals suffering from functional seizures with that of individuals who didn’t have seizures but might be suffering from mental health disorders like depression and anxiety.
The findings of the analysis revealed that those with functional seizures experienced thinning of their superior temporal cortex. This change in the brain structure impairs one’s control over his/her actions and reduces the person’s cognitive awareness. Thinning of the superior temporal cortex also alters the thickness of the patient’s left occipital cortex. For those who don’t know, the left occipital cortex of our brain is responsible for processing various sensory information including visual information.
The discussed changes were not noticed in patients, who didn’t experience functional seizures and were only suffering from mental health issues such as obsessive-compulsive disorder (OCD), anxiety, or depression.
One of the co-authors of the study Nicholas Beimer stated that this study points out how looking at standard tests like MRI more carefully can help doctors in identifying clues that can help them in making the right diagnosis. He added that this study should be used for improving diagnostic accuracy and speed to ensure that individuals suffering from functional seizures get the best treatment at the right time.
We at SepStream® put in our best efforts to ensure that our clients have access to the most advanced technology for streamlining various medical procedures. Our intuitive, AI-integrated software solutions are designed to help in diagnosis, treatment, as well as caregiving.