James Udelson is an MD and chief of the cardiology division at the Tufts Medical Center. He is also a professor of medicine and the director of nuclear cardiology at the same institution.
Udelson shared his understanding of the ‘Precise Trial’ conducted during the meeting of the “American Heart Association Scientific Sessions” in 2022. He was one of the investigators of the study.
According to the analysis, the extent of the composite of death and the need for algorithms for diagnostic catheters turned out to be 70% lower than the traditional approach testing method for patients without CAD (Unobstructive Coronary Artery) and under personalized care.
The Old Vs. The New Method
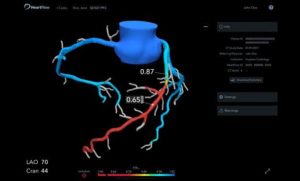
The study primarily focused on finding out the strategy most appropriate for evaluating patients who could have CAD. PRECISE aimed at comparing the care standard offered by the present setup with the latest Fractional Flow Reserve CT (FFR-CT) and Computed Tomography (CT).
The traditional care standards included referring patients to a diagnostic angiogram, stress testing etc. the outcomes were pretty enlightening. The researchers found the combination of FER-Ct and CT to be a better way for offering personalized care to patients than the traditional method.
The Objections
Udelson clarified that during the precision strategy testing the researchers found a perceptible favorable effect signaling which was not associated with death change or considerable alteration in non-fatal MI.
On the flip side, the team of researchers also found a substantial difference in the invasive angiogram numbers for patients who did not have obstructive CAD.
He further added that the new trial supplied more data to support FFR-CT and cardiac CT for the Chest Pain Evaluation Guidelines published by AHA/ACC in 2021. This made CCTA a reliable evaluation method for chest pain.
The guidelines also recommended using FFR-CT. the American Society of Nuclear Cardiology criticized the guidelines and dismissed FFR-CT as a reliable method due to the absence of huge trail data.
CCTA also got subjected to the complaint that it lacked sufficient physiological data establishing the importance of lesions seen on CT on hemodynamic flow.
The Solutions
To the first issue, Udelson gave a convincing answer. After the new trials, the researchers can offer random trial data which the ASNC considered essential.
Therefore, the previous doubts about the application of FFR-CT no longer qualify to prevail.
Udelson countered the second complaint as well. Based on the outcomes of the latest trials, the team suggested that non-invasive FFR-CT provides the supportive data needed to understand whether a patient qualifies for catheterization or not.
As a result, the number of patients unnecessarily undergoing the process of catheterization got reduced. This was true for the patients without obstructive Cad and all others as well. Udelson further added that the number of patients going for revascularizations also got better.
The Expert Suggestions
Udelson, who has used FFR-CT for many years, further mentioned that this method is ideal only when seeing physiological data remains critical. Using it for all patients is not something he suggested or thought necessary. Therefore, figuring out the patients who would need to go to the catheter lab becomes easier with FFR-CT.
When Pamala Douglas presented the data at the AHA session as one of the primary investigators, she claimed it to be quite convincing. Pamala Is an MD and works as the Ursula Geller Professor for Research at Duke University School of Medicine’s cardiovascular Disease department.
According to Douglas, the precision strategy is undoubtedly a reliable method for patients with continuous symptoms of coronary artery issues. She further elaborated that PRECISE helps evaluate the conditions of suspected CAD patients through a process of defined care pathways and testing.
Ron Blankstein is an MD and works as the cardiovascular imaging program’s director at Brigham and Women’s Hospital. He is also the director of cardiac CT there and co-authored the chest pain guidelines issued in 2021. Ron also discussed the PRECISE trial effects at the AHA late-breaking session.
According to him, coronary CT has drastically changed a physician’s capacity to see the arteries. He further added that since the trial follows the AHA guidelines regarding chest pain, it could be helpful in devising the next set of guidelines.
Ron and Udelson further noted that the trial led to an improvement in the life quality of patients by reducing the requirement of unnecessary angiograms for diagnosis. Additionally, the trial also helps boost the efficacy of diagnostic pathways by integrating FFR-CT with CT.
However, the team of researchers is looking forward to having more detailed follow-up data related to multiple patient cohorts covering a long time.
Technology has taken a leap in the last decade and the medical care sector is now in a better position in terms of diagnostic capabilities. At SepStream®, we understand the importance of staying abreast of the latest innovations and technology. Our list of AI-integrated software solutions makes diagnostic procedures faster and more accurate.